In a white lab coat and blue latex gloves, Neda Vishlaghi peers through a light microscope at six milky-white blobs. Each is about the size of a couscous grain, bathed in the pale orange broth of a petri dish. With tweezers in one hand and surgical scissors in the other, she deftly snips one tiny clump in half.
When growing human brains, sometimes you need to do some pruning.
The blobs are 8-week-old bits of brainlike tissue. While they wouldn’t be mistaken for Lilliputian-sized brains, some of their fine-grained features bear a remarkable resemblance to the human cerebral cortex, home to our memories, decision making and other high-level cognitive powers.
Vishlaghi created these “minibrains” at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, where she’s a research assistant. First she immersed batches of human pluripotent stem cells — which can morph into any cell type in the body — in a special mix of chemicals.
The free-floating cells multiplied and coalesced into itty-bitty balls of neural tissue. Nurtured with meticulously timed doses of growth-supporting ingredients, the cell clumps were eventually transferred to petri dishes of broth laced with Matrigel, a gelatin-like matrix of proteins.
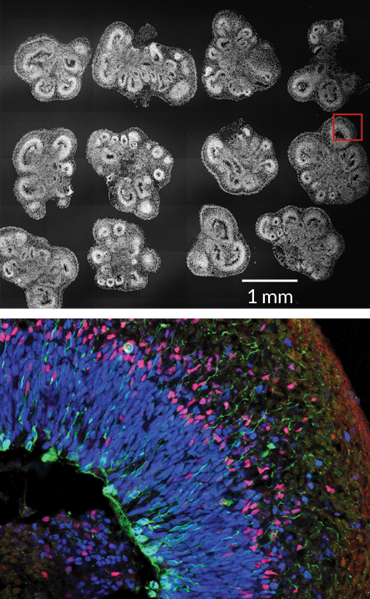
On day 56, the blobs display shadowy clusters of neural “rosettes.” Under a laser scanning microscope, razor-thin slices of those rosettes reveal loose-knit layers of a variety of dividing neural stem cells and the nerve cells, or neurons, they give rise to. The layered structures look similar to the architecture of a human fetal brain at 14 weeks of gestation.
“It’s like making a cake: You have many different ways in which you can do it,” says Novitch, who prefers using the Japanese method with a few tweaks. “There are all sorts of little tricks that people have come up with to overcome some of the common challenges.”
For instance, because the brain blobs lack a built-in blood supply, they must absorb enough oxygen and nutrients from the tissue-culture broth to remain healthy. To help, some labs circulate the broth around the tissue clumps. The UCLA researchers choose instead to grow theirs at higher oxygen levels and chop the blobs at the 35-day mark, when they are as wide as three millimeters, and then about every two weeks after. Sounds radical, but the slicing gives cells on the inside — some of which start dying — exposure to much-needed oxygen and nutrients. Those divided bits then continue growing separately. But cutting can be done only so many times before the expanding rosette structures inside are damaged.
With all the experimenting, researchers have cooked up a lot of innovations, including some nifty progress reported in just the last year. Scientists have concocted tiny versions of several brain regions ranging from the hypothalamus, which regulates body temperature, thirst and hunger, to the movement-controlling basal ganglia. Electrical chatter among neurons, reflecting active brain circuits, has been detected. And research groups have recently begun linking bits of specific regions like Legos. Scientists have even observed some early developmental processes as they happen within the human brain blobs.
The work is part of a broader scientific bonanza that comes from coaxing human stem cells to self-assemble into balls of organlike tissue, known as organoids, that are usually no bigger than a lentil. Although the organoids don’t grow enough to replicate entire human organs, these mini-versions can mimic the 3-D cellular infrastructure of everything from our guts to our lungs. That’s something you can’t get from studies of rodents, which have different biology than humans do.
Mini-organ models promise enormous advantages for understanding basic human biology, teasing apart human disease processes, and offering an accurate testing ground for finding or vetting drug therapies. And by creating personalized organoids from the reprogrammed cells of patients, scientists could study disease in a very individualized way — or maybe even use organoid structures to replace certain damaged tissues, such as in the liver or spinal cord.
Methods for making bits of brainlike tissue tap the innate tendency of human pluripotent stem cells to form neural tissue. Here’s one group’s process.
Day 0: Around 9,000 stem cells are transferred into V-shaped wells and suspended in a cocktail of vitamins, amino acids and (for the first six days) Y-27632, a chemical to prevent the stem cells from committing suicide. Within a few days, the multiplying cells self-aggregate into tiny balls of neural tissue. The broth is refreshed every two to three days.
Day 18: The enlarging neural balls are moved into petri dishes of broth with CDLC, a supplement that provides fats. High oxygen levels (40 percent oxygen, 5 percent carbon dioxide) help the tissue absorb enough oxygen. Well-defined clusters, or rosettes, show early layers of various types of developing neural cells by weeks four to five.
Day 35: At 2 to 3 millimeters wide, the brainlike organoids are cut in half to give cells inside more access to nutrients and oxygen. The tissue clumps are nurtured in new broth infused with growth enhancers: a gelatin-like matrix of support proteins called Matrigel, B27 vitamin supplement, heparin and the growth promoter LIF.
Day 56: Organoids are again snipped in half and transferred to new petri dishes made of oxygen-permeable plastic to optimize access to oxygen for healthy growth. From here on, the organoids are halved every two weeks or so, routinely surviving as long as 150 days.
Source: M. Watanabe et al/Cell Reports 2017
But the research is still in its early days. Although there’s been exciting headway, studies sometimes overstate the extent to which human brain organoids reproduce features of actual developing brain tissue, says stem cell biologist Arnold Kriegstein of the University of California, San Francisco. The minimodels still lack many basic components, including certain cell types, a blood-vessel network and inputs from other neural regions.
Another stumbling block is that brain organoids can vary a lot from protocol to protocol, or even batch to batch within the same lab. “The major focus now needs to be on reproducibility, and being able to get an approach that you can rely on to give you the same outcome each time,” Kriegstein says.
DIY organs
For decades, biology research has relied on cell lines grown in flat sheets in petri dishes, but those sheets lack the structural complexity of living tissue. Then came pioneering work that unveiled the do-it-yourself magic of stem cells raised free-floating in broth.
Organlike tissue bits can be generated from pluripotent stem cells that are either plucked from embryos or created by taking a person’s adult skin or blood cells and chemically inducing them to revert to an embryonic-like state. Starting in the mid-2000s, Yoshiki Sasai’s team at the RIKEN Center for Developmental Biology in Kobe, Japan, demonstrated how to grow brainlike structures using embryonic stem cells, first from mice and then humans.
In cross sections of 8-week-old brain organoids (top row), loose-knit cell layers roughly resemble the tighter bands in 14-week-old human fetal brain tissue (bottom row). The last column shows a zone of neural progenitor cells (red) and an outer layer of neurons (green).
Meanwhile, biologists elsewhere were whipping up other types of organoids, starting instead with adult stem cells. These rare, damage-repairing cells are found in many organs (including the brain), but the cells can transform into only a limited range of cell types. In 2009, Hans Clevers of the Hubrecht Institute in Utrecht, the Netherlands, announced that his lab unexpectedly
created a miniature version of a gut while cultivating adult stem cells that the team had discovered in mouse intestinal tissue. Grown in a drop of Matrigel with a trio of growth-inducing factors, these cells coalesced into little spheres containing tiny projections that resembled the fingerlike villi that absorb nutrients in the gut.
Scientists soon were concocting tiny
facsimiles of human stomachs, livers, kidneys, lungs and more (
SN: 12/28/13, p. 20). “We essentially are discovering the vitality of what the stem cells actually do,” says Clevers, who is president of the International Society for Stem Cell Research. “We give [the cells] a little push, and they do whatever they’re good at.”
The trick is knowing exactly which ingredients to use to make different organs. For pluripotent stem cells, that means exposing them to just the right growth factors or inhibitors at just the right times, over about a month, says James Wells of the Center for Stem Cell and Organoid Medicine at Cincinnati Children’s Hospital Medical Center. Some of those essential instructions are well-known from decades of research on embryo development in fish, chickens and rodents; the same chemical cues generally work for all animals with spinal cords, including people.
Under a microscope, rosettes of neural cells are visible along the perimeter of an 8-week-old brain organoid. The center, where cells have died, is dark.
However, for many body parts, organoid makers must suss out recipe instructions from scratch. Working with Jorge Múnera and other colleagues, Wells recently produced a minimodel of a human colon using human induced pluripotent stem cells. But first, the team conducted months of experiments on frog and mouse embryos to identify the signals for forming a colon. “It took a while to figure out what the special sauce was,” Wells says.
Some scientists have distant dreams of using organoid methods to grow full-size livers or kidneys in the lab for transplantation. A more attainable goal may be regenerative tissue transplants, for example, replacing dying liver cells in someone with early-stage liver disease with chunks of healthy stem cells from a personalized liver organoid. Or, in patients who’ve had part of the small intestine removed, tiny pieces of gut organoid tissue could be implanted and, after growing larger, connected to the intestine.
Head games
The human brain, meanwhile, is vastly more complicated than any other organ. It’s unlikely that scientists will ever be able to build a full replica. While the initial brain-making recipes were stunning for what they could achieve, they left much room for improvement. In the years since the 2013 debut of human brain organoids, research groups have worked to grow bigger brain tissue clumps and more uniform structures.
The Austrian method for making whole-brain organoids, in particular, produced a random mix of neural regions laid out in a topsy-turvy manner. But bioengineering tricks may help. In a study last year, Lancaster, now at the MRC Laboratory of Molecular Biology in Cambridge, England, and Knoblich got more consistent results
by adding polymer filaments as scaffolding to guide the organization of the minibrain models.
With surgical scissors, a UCLA biologist prepares to snip one of those organoids in half to give inner cells more access to oxygen and nutrients from the broth in the dish.
Other scientists, following the Japanese approach, which generally gives more predictable results, have concentrated on coaxing out specific cell types or structural features of the real brain. For instance, one constraint is that the organoids form slowly, more or less sticking to the same timeline of development as does a human brain during gestation. But without a blood supply, growth is limited; the brain bits reach only a few millimeters in size. That means organoid models are often short on cell types from later development stages, such as cells called astrocytes. These star-shaped cells are crucial for creating and curating the connections between neurons, and also may help with forming memories (SN Online: 11/15/17).
Astrocytes don’t fully mature in a baby’s brain until after birth. But Stanford University neuroscientist Sergiu Paşca has crafted a method for making and maintaining 4-millimeter-wide balls of human cortex–like tissue (he calls them spheroids) in 3-D culture for an extended time. Last August in
Neuron, his team described
organoids that survived for more than 20 months — long enough, analyses showed, for astrocytes to mature and function in ways that mimic their real-brain counterparts.
Of great interest, also, are the outer radial glial (oRG) cells, neural stem cells that are pivotal for constructing the unusually big cortex that’s unique to humans; oRG cells are scarce in mouse brains. When Novitch’s lab group at UCLA tried the original Japanese and Austrian organoid-making recipes, the output of oRG cells was underwhelming. So Novitch worked with Vishlaghi and postdoctoral researcher Momoko Watanabe to refine the protocol to pump up the cells’ production and reliably generate better cerebral blobs.
Among other tweaks, Novitch’s team added a dash of a molecule dubbed LIF, which recent studies by others had suggested can spur the oRGs to multiply. It worked, leading to a threefold increase in the oRG populations and enhanced growth of upper neuron layers. The researchers shared
their revised protocollast October in
Cell Reports.
Helping hand
Neural stem cells called outer radial glial (oRG) cells help fuel the expansion of the unusually big human brain. A growth factor called LIF tripled the number of oRG cells in growing minibrains by week 12.
Applying a growth factor to mini brain models
Source: M. Watanabe et al/Cell Reports 2017
On a different front, labs have begun assembling more complex minibrain models, like playing with self-directed Legos. For two months, Paşca’s team at Stanford grew spheroids in separate sets of dishes that mimicked either cortex tissue or an adjacent underlying region known as the subpallium. Then the researchers put the different bits side-by-side and left them overnight in a culture tube. Similar to how the two regions normally connect in the developing brain, the little pieces knew what to do. “By the next day they are essentially fused to each other,” says Paşca, who announced the results in May in Nature.
During the fusion process, the researchers took time-lapse videos of long, spaghetti-like cells called interneurons migrating from a spheroid of the subpallium into a cortexlike spheroid.
“They don’t crawl, they actually jump,” Paşca says. The images capture aspects of a hallmark phenomenon that normally unfolds during the second and third trimester of fetal gestation.
Testing ground
Once on the other side, interneurons form a circuit with — and quell the activity of — excitatory neurons in the cortexlike tissue, electrophysiological tests suggest. If not quieted, excitatory neurons will trigger neighboring cells to fire. In the real brain, maintaining a proper balance in neural network activity is important; disruptions in it appear to foster disorders such as epilepsy, and perhaps schizophrenia and autism.
Indeed, in the same paper, the Stanford team reported new discoveries using personalized brain spheroids derived from induced pluripotent stem cells of
patients with Timothy syndrome — a rare condition caused by an overactive calcium channel found mainly in the brain and heart. Patients with the disorder have epilepsy, autism and heart problems. In the patients’ spheroids, interneurons migrated inefficiently but, by adding drugs that blocked the dysfunctional calcium channel, the researchers could reverse the problem. The brain organoids made these intriguing observations possible, Paşca says. “We couldn’t have done this in any other way.”
Stunted
A brain organoid infected by Zika virus at 28 days old is severely stunted two weeks later (right) compared with a healthy organoid of the same age (left).
When sliced open, at higher magnification, a healthy cortexlike organoid (left) shows normal structure: a rosette with visible cavity in the middle, neural stem cells (red) and neurons (green and blue). A Zika-infected organoid (right) shows collapse of the rosette, with fewer neural stem cells and neurons.
Organoid experiments by others have, meanwhile, helped confirm that the Zika virus targets and kills oRG cells and other neural precursor cells, contributing to small brain size in infected infants.
In a 2016 study, Johns Hopkins University neuroscientists Guo-li Ming and Hongjun Song reported on their own techniques for
creating brain bits that have a well-defined zone of oRG cells. After infecting these organoids with the Zika virus, the researchers
observed a collapse of cortexlike tissue that may partly explain the stunted brain growth (
SN: 4/2/16, p. 26). 2-D cell-culture and mouse experiments also provided key evidence of the virus’s modus operandi; although the rodent brain doesn’t harbor the full contingent of human neural stem cells, it has blood vessels and immune-system components that organoids lack.
In search of Zika-fighting treatments, Ming and Song, both now at University of Pennsylvania, and their colleagues have been screening thousands of compounds in 2-D cell cultures, and then validating the most promising candidates with tests in 3-D brain organoids. The team has found several potential antiviral and neuron-protecting agents to pursue. Novitch’s UCLA lab group has likewise used its brain organoids to pinpoint additional receptors by which the virus may gain entry into neural stem cells, and identified a few other drug leads for blocking infection.
Organoids may also prove valuable for tailoring treatments for patients, says David Panchision, chief of the developmental neurobiology program at the National Institute of Mental Health in Bethesda, Md. Researchers might generate personalized brain organoids from the reprogrammed skin cells of individuals with, say, schizophrenia and test which medications work best for patients with particular genetic profiles of the illness.
In the Netherlands, based on research reported in 2016 in
Science Translational Medicine, Clevers and colleagues
are already using personalized gut organoids, derived from rectal biopsies, to test whether cystic fibrosis patients will benefit from available drugs. Tailored regenerative therapies with 3-D substructures of neural tissue may also be possible, Panchision adds, for conditions like Parkinson’s disease or spinal cord injury.
Blocking infection
Images show 4-week-old brain organoids with no infection (left) and with Zika infection (middle, virus is green, dead stem cells are pink). Treatment with the drug duramycin before exposure to Zika largely staves off infection and cell death (right).

Growing pains
For now, though, scientists have hefty challenges to overcome. Much work remains in optimizing how faithfully the bits of tissue reproduce normal brain function and architecture, Panchision says. For one thing, the organoids are developmentally young and don’t reflect a mature brain. And researchers must figure out how to build in some core features: the necessary blood vessels, immune-system cells called microglia and connections from other brain regions, such as the thalamus and cerebellum. Not to mention steroid and thyroid hormones, which also shape brain growth.
However, scientists don’t necessarily need or want to create a comprehensive replica of the human brain in a dish, Panchision and others point out. Rather, the goal is to build robust and reliable models for studying specific aspects of brain function.
Thus the pressing need for standardized, reproducible organoid-making recipes. Novitch’s group and many other labs are still trying to figure out why the brain bits can vary so much in size, composition and structure. Part of the trouble is the ingredients: Subtle variations in tissue-culture chemicals and Matrigel, or in different stem cell lines and how they are grown first in 2-D culture, can have a big impact on how the organoids turn out, Novitch says.
At the same time, researchers need to do a more thorough job of analyzing brain organoids to know what’s actually in them at different developmental time points, compared with actual human fetal brain tissue, says UCSF’s Kriegstein. It’s otherwise hard to say whether a brain blob truly recapitulates the neural tissue that scientists claim it does. Labs have started tackling the problem with a tool called single-cell transcriptome analysis, which gives readouts of all the genes that are active in individual cells.
“Greater rigor is needed,” Kriegstein says. “And I am sure we will eventually get there.”
This story appears in the March 3, 2018 issue of Science News with the headline, "Brain-making 101: Self-assembling clumps bring a dose of 3-D reality to studies of human organs."
Citations
M. Watanabe et al.
Self-organized cerebral organoids with human-specific features predict effective drugs to combat Zika virus infection.
Cell Reports. Vol. 21, October 10, 2017, p. 517-532. doi:10.1016/j.celrep.2017.09.047.
E. Di Lullo and A.R. Kriegstein.
The use of brain organoids to investigate neural development and disease.
Nature Reviews Neuroscience. Vol. 18, October 2017, p. 573. doi:10.1038/nrn.2017.107.
S. A. Sloan et al.
Human astrocyte maturation captured in 3D cerebral cortical spheroids derived from pluripotent stem cells.
Neuron, Vol. 95, August 16, 2017, p. 779. doi:10.1016/j.neuron.2017.07.035.
J. O. Múnera et al.
Differentiation of human pluripotent stem cells into colonic organoids via transient activation of BMP signaling.
Cell Stem Cell, Vol. 21, July 6, 2017, p. 51. doi:10.1016/j.stem.2017.05.020.
M. A. Lancaster et al.
Guided self-organization and cortical plate formation in human brain organoids.
Nature Biotechnology. Vol. 35, July 2017, p. 659. doi:10.1038/nbt.3906.
F. Birey et al.
Assembly of functionally integrated human forebrain spheroids.
Nature. Vol. 545, May 4, 2017, p. 54-59. doi:10.1038/nature22330.
X. Qian et al.
Brain-region-specific organoids using mini-bioreactors for modeling ZIKV exposure.
Cell, Vol. 165, May 19, 2016, p. 1238. doi:10.1016/j.cell.2016.04.032.
M.A. Lancaster et al.
Cerebral organoids model human brain development and microcephaly.
Nature. Vol. 501, September 19, 2013, p. 373. doi:10.1038/nature12517
T. Kadoshima et al.
Self-organization of axial polarity, inside-out layer pattern, and species-specific progenitor dynamics in human ES cell-derived neocortex.
Proceedings of the National Academy of Sciences. Vol. 110, December 10, 2013, p. 20284. doi:10.1073/pnas.1315710110.
T. Sato et al.
Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche.
Nature. Vol. 459, May 14, 2009, p. 262. doi:10.1038/nature07935.